Understanding Vaginal Discharge
Even though the word may give some of us the ‘ick’, discharge isn’t gross and you shouldn’t be embarrassed to talk about it! In fact, your discharge can tell you quite a lot about what’s going on in your body! Vaginal discharge is a bit like a coded message. It can help you to discover more about your menstrual cycle, whether you could have an infection, or even if you could be entering through perimenopause or menopause.
Having discharge is completely normal, and it shouldn’t be a cause for concern, but on occasion the smell or texture of your discharge may indicate that you have an infection and should seek support.
It’s important to know which signs should set off alarm bells, so you can see your doctor and get on top of symptoms. So, keep scrolling and we’ll explain to you how to crack the code so you’ll know exactly what’s going on with your discharge downstairs!
The basics of vaginal discharge
Vaginal discharge (or just discharge) is the fluid that our vaginas produce in order to keep our vaginas and vulvas clean and healthy. The amount of discharge you produce can vary on a daily basis, and these changes shouldn’t usually be a cause for concern. If you notice any changes to the color, quantity, texture, or smell of your discharge however, you should make an appointment to see your doctor.
What is the purpose of discharge?
Vaginal discharge (or just discharge) usually contains mucus, bacteria, and old skin cells. We start producing discharge at puberty, and it:
- keeps us lubricated to prevent irritation
- helps our bodies to remove waste
- shields our bodies against germs that try to enter through the vagina
How much discharge should I produce?
You should generally have 2-5mL of clear or white discharge exiting your vagina everyday– this is about the same as ½ – 1 teaspoon of fluid.
You should also expect your discharge to be odorless, or smell a little sweet, sour, or tangy. However, there are plenty of reasons why you might notice different quantities, colors, and textures of discharge downstairs.
For one, the quantity and texture of discharge can vary from person to person, if you’re dehydrated, or at a certain point in your menstrual cycle. The characteristics of your discharge are also impacted by hormones such as estrogen.
Having higher levels of estrogen is associated with producing more discharge, and lower estrogen levels are associated with less discharge.
This is why you might notice more discharge when you’re ovulating, right before your period, or if you’re taking medications such as hormonal birth control.
It’s also why women who are going through perimenopause and menopause may feel dryer downstairs.
Should I be worried about my discharge?
Changes in discharge that appears different from the cyclical changes you usually notice throughout your menstrual cycle can in some case be due to sexually transmitted infections (STIs), or other conditions.
Regardless of why, changes to your discharge is your body’s way of sending out an SOS, and you should seek medical attention pronto!
Comparing colors, smells, and consistencies
If you’re reading this and wondering exactly which changes in your discharge you need to watch out for, I’ve got you covered! The following infographic shows how your discharge may look and smell when you’re healthy, as well as when you may be in need of some additional support from your provider.

The colors and consistencies of your discharge change as a result of shifts in the makeup of bacteria, fungi, and fluids that make them up. If this sounds familiar, you may have read our previous post about finding your perfect pH!
Our discharge can reflect changes in our vaginal microbiomes. For instance, if you notice that your discharge has a pink tinge, it could be because blood has been added to the mix of bacteria, mucus, and old skin cells that generally make up your discharge.
The tricky part here can be figuring out why there’s blood in your discharge. There are dozens of possible reasons for this, ranging from implantation-related bleeding in early pregnancy, to sexually transmitted infections (STIs) such as chlamydia and gonorrhea, and even rough sex.
With all the situations and conditions that can affect your discharge, it’s a good thing that there are trained professionals that you can consult for advice and treatments!
Take (dis)charge of your vulvo-vaginal health!
Whether you notice an unfamiliar smell, a concerning color, a curious texture, or even a shift in the quantity of discharge coming from your vagina, you should see your doctor.
Your primary care provider will be able to help you decode your discharge and decide whether you need treatment for the changes you’ve been experiencing.
You should also consider going to see them in person instead of having a telehealth appointment. In order to make the most accurate judgements, your doctor will want to get a good sense of the changes in your discharge that are worrying you, as well as any other symptoms that you may be experiencing. This means that they may want to see your discharge themselves, and even take a sample of your discharge to test for certain germs.
It’s particularly important to get medical attention when you notice changes in your discharge because many of the conditions that cause changes in the appearance and smell of discharge are quite serious and don’t just go away on their own.
Is it bacterial vaginosis (BV) or vaginal thrush?
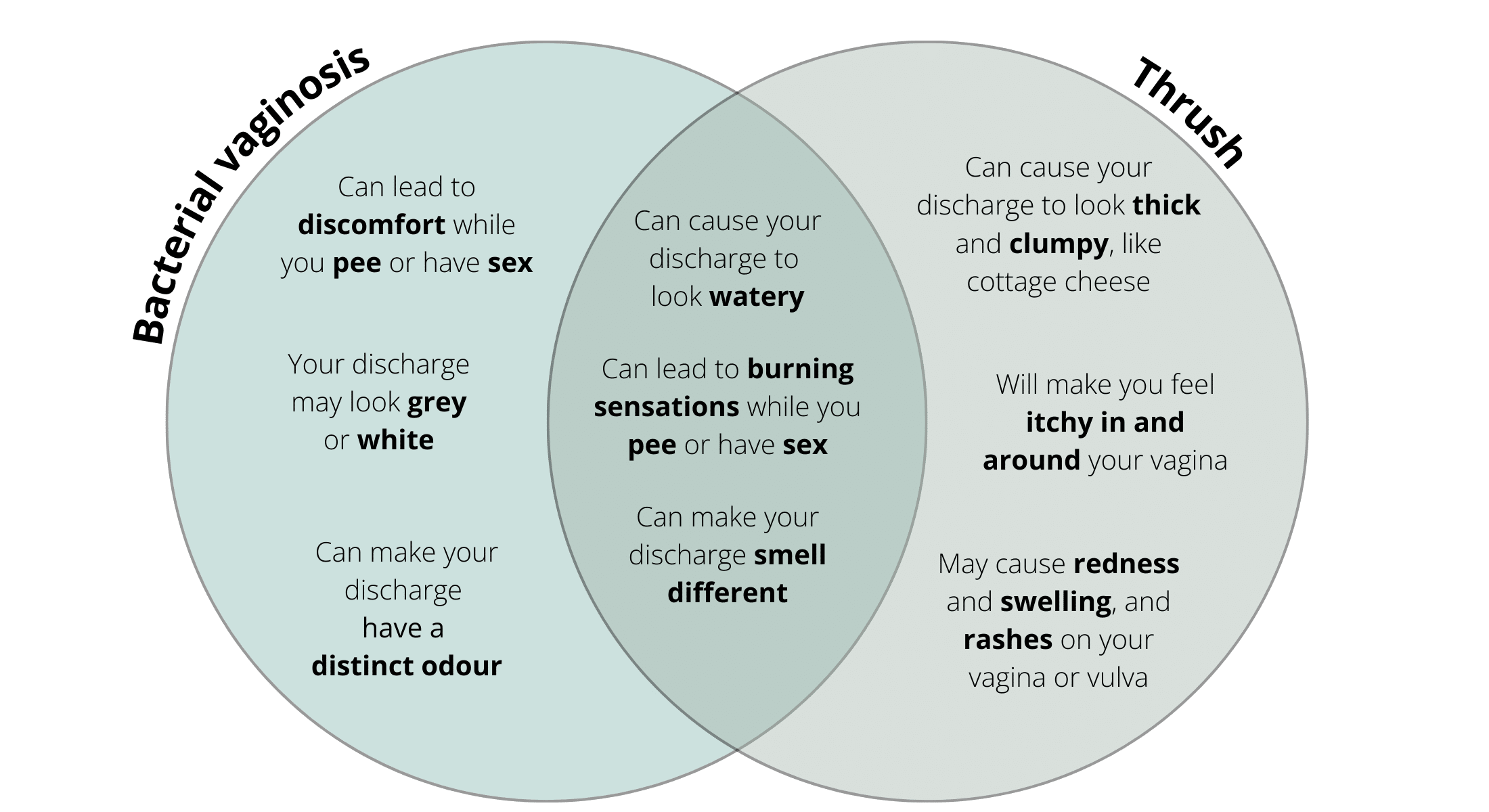
BV and vaginal thrush are both conditions that cause discomfort to millions of women every year, and a telltale symptom of both is a change in the appearance and smell of discharge. In fact, many women mistake BV for thrush, which unfortunately can lead to more problems down the line.
BV is an infection that you develop when there’s too much of certain bacteria in your vagina, while thrush is the result of too much of a certain fungus downstairs. This means that they require very different treatments, and those of us who mistake our BV for thrush may extend the length or severity of our infections by treating our condition with medications other than the ones that we should be using.
If you’re wondering how you can spot the difference between BV and thrush, I hope that this Venn diagram will help.
The Symptoms of BV vs Thrush
If you do in fact have thrush, or you think you may, you should see your doctor so they can help you confirm your suspicions and give you advice about treatments and preventative measures for the future. If this isn’t your first rodeo, you can also re-up on your go-to over-the-counter (OTC) anti-fungal medication in the pharmacy section at your local drug store.
Otherwise you should get yourself to the doctor as soon as you can, as you’ll need a prescription to relieve BV symptoms with antibiotics. You should also make sure to take the full course of medications that your doctor prescribes because about half of us will see our symptoms return within a year of our initial infection, and missing even one dose can increase the chances that BV will come back to bother you in the future.
Listen up, your discharge wants to tell you something!
In many ways, your discharge is an extension of your body, and in addition to the important work it does to protect you from irritation and germs, it does a great job of showing you what’s going on in your vagina and vulva.
So, listen to what your discharge is telling you! Don’t be afraid to get in there and really take a look and examine how your discharge is looking, smelling, or feeling. Equally, don’t be embarrassed to bring up your concerns with your doctor.
We all have discharge, and we can all experience changes to our discharge that cause us discomfort. Your doctor will be the best person to help you find relief, and being open and honest with them is the best way to figure out what the problem is and find the solution.

References
Amrin SS, Lakshmi GJ. Vaginal discharge: The diagnostic enigma. Indian J Sex Transm Dis AIDS. 2021;42(1):38-45. doi:10.4103/ijstd.IJSTD_92_18
Bishop GB. Vaginal Discharge. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990.
Dorjey Y, Wangmo D, Tshomo D. Assessment of excessive vaginal discharge among women who presented to Phuentsholing General Hospital: A hospital-based study. Health Sci Rep. 2022;5(5):e793. Published 2022 Sep 1. doi:10.1002/hsr2.793
The American College of Obstetricians and Gynecologists. FAQ: How to prevent sexually transmitted diseases [internet]. Washington DC: American College of Obstetricians and Gynecologists; 2020. [cited 2022 May 9]. Available from https://www.acog.org/womens-health/faqs/how-to-prevent-stis
The American College of Obstetricians and Gynecologists. FAQ: Vulvovaginal health [internet]. Washington DC: American College of Obstetricians and Gynecologists. Reviewed Jan. 2022. [cited April 26, 2022]. Available from https://www.acog.org/womens-health/faqs/vulvovaginal-health#:~:text=Vaginal%20dryness%20can%20be%20caused,and%20urinary%20tract%20during%20menopause.
Sim M, Logan S, Goh LH. Vaginal discharge: evaluation and management in primary care. Singapore Med J. 2020;61(6):297-301. doi:10.11622/smedj.2020088
Watson WJ, Demarchi G. Vaginal discharge: an approach to diagnosis and management. Can Fam Physician. 1987;33:1847-1852.





