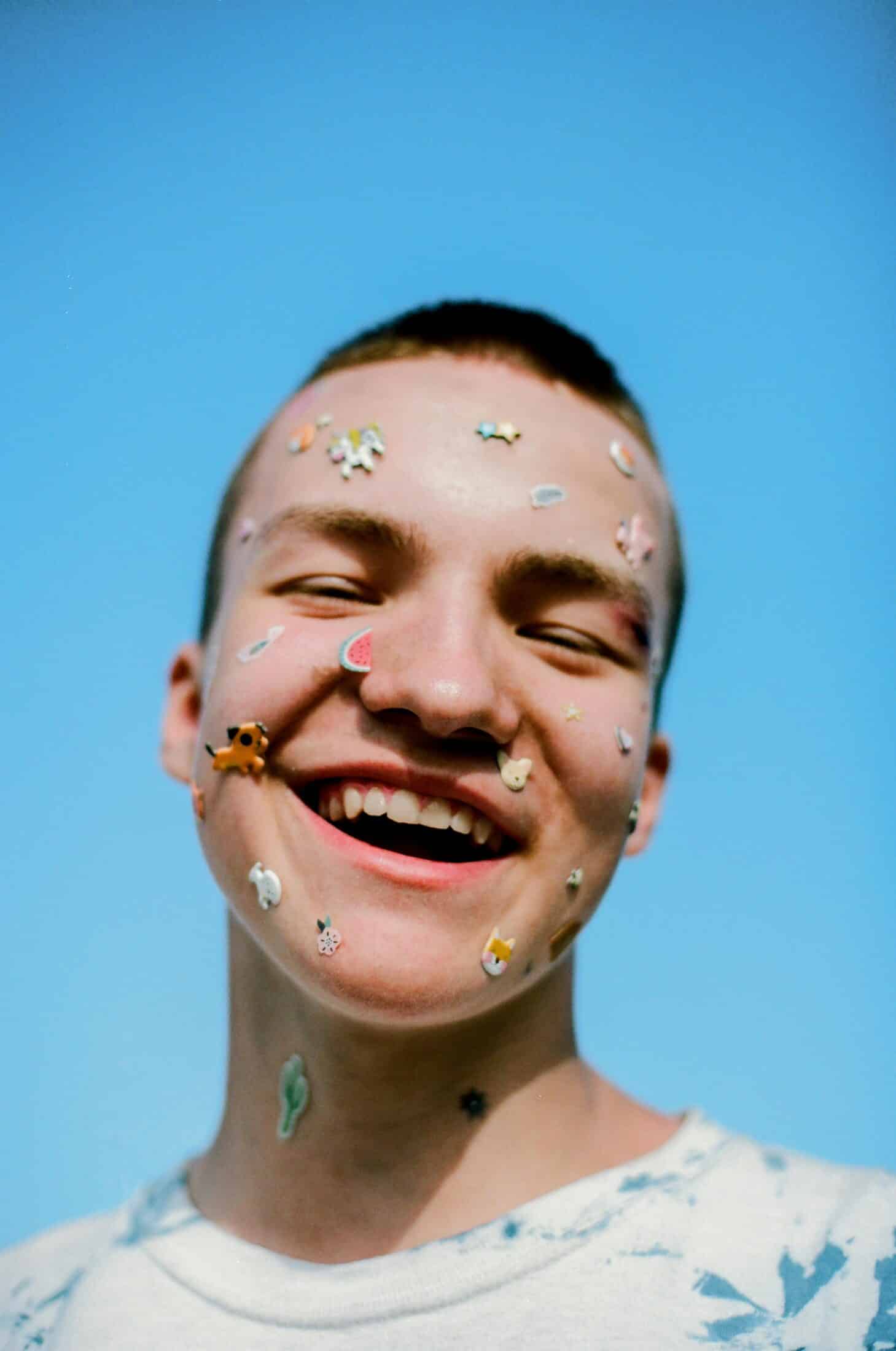
Happy Pride month!
If you haven’t listened to our recently released podcast episode yet, check it out here!
Hormonally’s Executive Director, Lauren, had a chat about the experiences of transgender and non-binary (NB) folk navigating perimenopause and menopause with Dr Hammond – an endocrinologist based in the UK with extensive experience in treating symptoms of gender dysphoria.
In recording this episode, the Hormonally team realized just how little guidance is available when it comes to navigating Gender Affirming Care (GAC) in the US. As a result, we decided we wanted to do our bit to help ‘bridge’ that gap for anyone who may be feeling overloaded. Our hope is to help turn your quest toward learning about gender affirmation from exhausting to exciting! Whether you‘re starting to explore your gender identity, you don’t know what steps to take to seek medical intervention, or you just want to learn more about how to be an informed ally, this guide is for you.
For those seeking guidance, we hope this blog post will support you to feel confident on your journey toward receiving gender-affirming care (GAC).
GAC needs GPS
Navigating GAC in the Global North is a complex process for many. Prioritizing improvements in access is essential because GAC is recognised as something that can impact the psychological well-being of millions of gender diverse people living in the US.
Increasingly, clinicians report not feeling equipped to answer questions about gender-affirming needs, but this begs the question, where are trans and NB folk supposed to turn to find guidance if not their healthcare provider?
The Basics
Here are some terms to keep handy while learning about gender affirmation:
Gender identity is our internal concept of our gender, whether that matches the sex we were assigned at birth, or not.
Gender expression is the expression of one’s gender identity; for lots of people this is expressed by characteristics such as hair, clothing, voice deepness, etc.
Gender affirmation encompasses the actions we take to help align our lived experience with the gender identity that feels the most authentic to us. This is a very broad concept, and can include medical, social, and legal processes.
Gender dysphoria is the feeling of unease or distress we have if we feel our gender identity or expression does not align with the way we present (how we are perceived by others).
Gender euphoria is the feeling of joyful security we feel when affirmed in our gender.
Where do we even start?
Affirming our gender can be a lifelong process and the way we see ourselves and feel about our gender identity can change over time.
Some great questions to begin asking ourselves about whether or not we feel good about our gender identity may include the following:
- Do I feel like my outward appearance and my body match how I feel on the inside?
- Do I wish that I was a different gender, or that I could present differently?
- How does it make me feel when someone uses pronouns and gendered or gender neutral terms like “mister”, “miss”, “he”, “she”, or “they” to refer to me?
If we don’t feel a sense of alignment between the way we look and feel, then there are a number of avenues we can take towards achieving gender affirmation.
Gender affirmation is not an organized or streamlined process. It’s important to remember that an abundance of options are available and it’s up to us to decide which, if any of these options are things we’d like to do.
The end goal of gender affirmation is feeling good about ourselves and living with the gender identity that feels most authentic to us. So this journey requires us to look inwards and check-in with ourselves often.
A great place to start on the journey of gender affirmation is to explore our gender identities with activities that don’t require the help of medical doctors or lawyers.

Step 1: Exploring our gender identities
Some things we can do to explore our gender identities include:
- Changing our hair and/or wardrobes
- Using different pronouns (“he”, “she”, “they”, etc.)
- Talking to a therapist or counselor
- Talking to supportive friends and family
- Vocal coaching
- Chest binding
We can check in with ourselves throughout this process by asking questions, including:
- What do I like and dislike about the things I’ve been trying during my gender identity exploration?
- Are there any other activities I would like to try, or conversations I would like to have?
- What would make me happier about my gender expression and the way I present?
It’s a good idea to journal or keep a record about our feelings throughout this process.
This is also a good time to start writing down our questions about GAC, the outcomes that we are looking to achieve, and even our fears and hesitations about the process.
Step 2: Exploring our care options
Once we have a better idea of the differences between the way we currently present and how we wish to present, we’ll likely also have a better idea of what types of medical care we would like to access.
Again, it’s possible that we won’t feel the need to access any gender-affirming medical care, but it’s good to know what our options are.
Medical interventions that we can access for gender-affirmation include gender-affirming hormone therapy (GAHT) and surgery.
GAHT
GAHT can be used to help alleviate symptoms of gender dysphoria, and involves using sex hormones to help masculinize or feminize our bodies.
Feminizing hormone therapy can be used to reduce levels of testosterone and increase levels of estrogen, while masculinizing hormone therapy can be used to reduce levels of estrogen, and increase levels of testosterone.
GAHT helps to address characteristics, like facial hair, body fat distribution, voice deepness, muscle mass, etc. Those undergoing masculinizing GAHT may also stop having periods after beginning to take medications.
Medications can be administered as injections, pills, skin patches, and gels.
Surgery
Gender-affirming surgeries can be used to help masculinize or feminize facial features, to reconstruct genitals, to reduce or augment breasts, and even to masculinize or feminize one’s voice.
Step 3: Getting GAC
Both GAHT and surgery require us to have a consultation with a medical doctor. For lots of trans and NB folk this can be a daunting idea. If we have not always felt that we have had our identity affirmed, seeking support can bring up many complicated feelings.
However, it’s important to remember that professionals working in this space are dedicated to supporting people to live comfortably as themselves.
Some care providers require a letter of “support” from a mental health professional before allowing us to start GAHT or undergo surgery, while others make their own assessment of our readiness to receive care by providing us with information and having conversations with us.
Care providers that use the latter method to approve GAC plans follow an informed consent model of care. This is a preferred model of care for many because it allows us to have a larger hand in decisions surrounding medications and dosages.
We also prefer this model of care because we don’t have to go through additional steps of getting a mental health professional to sign off on our bid for GAC.
Needing approval by a mental health professional is more in line with the standard model of care, in which we must first receive a diagnosis of gender dysphoria from a mental health professional. This is an undesirable option for many because it implies that being trans or gender-diverse is a mental-health issue that must be assessed by a professional, and also adds costs to our GAC plans and pushes back our timelines.
Considerations that both care providers and mental health professionals will take into account before approving a GAC plan include whether or not we’re experiencing feelings of gender dysphoria, and physical aspects of our health that can be assessed through bloodwork.
Once a care provider has approved our GAC plan, it’s time to fill that prescription or perhaps prepare for that surgery!
If we decide that GAHT or surgery is something that will help us achieve our gender-affirmation goals, then we’ll need to check in with our care providers occasionally throughout the process. At first, we’ll need to check in at monthly or quarterly intervals, with the frequency of visits changing as needed.
.
Considerations
These are some things that we should think about and discuss with loved ones or potential care providers when creating a treatment plan.
Care providers
To find out whether we can work with our current care providers to access GAC, we can use the following prompts to start a conversation:
- I’m exploring my gender identity and wanted to discuss your experience providing GAC.
- Would you be able to help me with my medical gender-affirmation?
- Do you know of any organizations or have any colleagues who are experienced in working with trans and gender-diverse patients?
We may find that they don’t feel equipped to help us with this aspect of our medical care. In this case, they may direct us to other providers, or we can seek them out ourselves.
It’s always important to remember that we have a right to ask to be signposted to a suitable provider if our current provider says they are unable to support your treatment goals.
For those of us who are looking for an experienced provider that’s close by, we can use this directory from the World Professional Association for Transgender Health.
Additionally, if we would specifically prefer to access care providers that work under the informed consent model of care, this map of informed consent clinics will come in handy.
Cost
How much does it cost to receive gender affirming care?
Unsurprisingly, it depends. According to a recently published study, the out-of-pocket cost of GAHT in 2018 was between $72 and & $3,792, while gender-affirming surgery could cost between $6,900 and $63,400.
These numbers can vary depending on where in the country we live, whether we do or don’t have insurance, and the extent of care that insurance providers cover.
Those who are interested in accessing funding assistance for their GAC can try non-profit organizations like Point of Pride and Genderbands.
While we understand it can be tempting to seek cost effective solutions, it’s important to avoid GAHT and hormone products we may come across on the internet. These products may be marketed as cheaper and accessible alternatives to the medications that we receive through our care providers, but products can be fake and harmful.
The only way we should be accessing GAC is through certified care providers.
Timelines
There are two timelines that we should be aware of if we’re thinking of accessing GAC.
- The time it will take from going to see our care providers about getting GAC, to actually beginning treatments. It can take a while to begin GAHT. Some care providers have long wait lists that can vary from a couple of months to a few years.
- The time it will take from starting treatments, to when we see results. Depending on the types of GAC we decide to access, the time it takes to start seeing results may differ. The effects of surgery can be seen as soon as our bodies heal from our operations. It can take as little as a month for us to start noticing differences in the way we look after starting GAHT, with changes being more pronounced the longer we’re on our medications.
Fertility
GAHT and certain gender-affirming surgeries can impact our ability to have children ourselves.
This isn’t necessarily a reason not to pursue GAC. However, it may be a reason to consider using fertility preservation techniques prior to beginning our care plans.
Some may consider freezing eggs, sperm, or embryos. Some may also consider waiting to receive treatments until after having children, or pausing treatments for a while. Some may even consider other routes to parenthood, such as adoption.
Mental Health
Seeking out and receiving GAC can be difficult. There can be stigmas associated with being trans and gender-diverse, and many obstacles must be overcome to begin treatments.
However, at the end of this road, we find the euphoria that comes with feeling affirmed in our gender identities. Overall, receiving GAC seems to positively influence our mental well-being.
For example, in a study comparing the mental health of trans and gender-diverse people, receiving gender-affirming surgery was associated with a 42% reduction in psychological distress and 44% reduction in suicidal ideation.
For most, the benefits of receiving GAC outweigh the costs and drawbacks by far.
The future of GAC?
Trans telehealth platforms have been gaining popularity in recent years.
These monthly subscription services are not necessarily a cost-cutting alternative to more traditional care providers, but they do allow users to go through the steps of accessing GAC on a much quicker timeline. They are often run by trans and gender-diverse community members, creating a more welcoming environment to users. They also share comprehensive information about the states that they can be accessed in, the insurance providers that they accept, and additional lifestyle information.

Where to find more information
Thank you for taking the time to read this guide! While the journey to gender-affirmation can be long and filled with obstacles, GAC is worth the trouble, as it can improve the quality of life and improve mental health outcomes of those who seek out care.
Having access to attainable and clear cut information is fundamental for supporting gender-diverse people, particularly in the initial stages of gender-affirmation.
We hope you’ve enjoyed this introduction to GAC, which can serve as a starting point for those who are new in the gender-affirming space.
For more information, we encourage interested readers to visit resources including Planned Parenthood and the National Center for Transgender Equality. Additionally, for those who would like to explore telehealth resources, Plume and FOLX Health are available and can provide readers with the A to Z of GAC .
In the words of America’s favorite drag queen, Ru Paul, “When you become the image of your own imagination, it’s the most powerful thing you could ever do”.
Happy Pride everyone, let’s live our best lives and become the version of us that we’ve always imagined!
References
Almazan AN, Keuroghlian AS. Association Between Gender-Affirming Surgeries and Mental Health Outcomes. JAMA Surg. 2021 Jul 1;156(7):611-618. doi: 10.1001/jamasurg.2021.0952. PMID: 33909023; PMCID: PMC8082431.
Baker K, Restar A. Utilization and Costs of Gender-Affirming Care in a Commercially Insured Transgender Population. J Law Med Ethics. 2022;50(3):456-470. doi: 10.1017/jme.2022.87. PMID: 36398652; PMCID: PMC9679590.
Bhatt N, Cannella J, Gentile JP. Gender-affirming Care for Transgender Patients. Innov Clin Neurosci. 2022 Apr-Jun;19(4-6):23-32. PMID: 35958971; PMCID: PMC9341318.
Cheng PJ, Pastuszak AW, Myers JB, Goodwin IA, Hotaling JM. Fertility concerns of the transgender patient. Transl Androl Urol. 2019 Jun;8(3):209-218. doi: 10.21037/tau.2019.05.09. PMID: 31380227; PMCID: PMC6626312.
McNamara M, Abdul-Latif H, Boulware SD, Kamody R, Kuper LE, Olezeski CL, Szilagyi N, Alstott A. Combating Scientific Disinformation on Gender-Affirming Care. Pediatrics. 2023 Sep 1;152(3):e2022060943. doi: 10.1542/peds.2022-060943. PMID: 37605864.
Meier AC, Papadopulos N. Lebensqualität nach geschlechtsangleichenden Operationen – eine Übersicht [Quality of life after gender reassignment surgery: an overview]. Handchir Mikrochir Plast Chir. 2021 Dec;53(6):556-563. German. doi: 10.1055/a-1487-6415. Epub 2021 Jun 16. PMID: 34134147.
Scheim AI, Baker KE, Restar AJ, Sell RL. Health and Health Care Among Transgender Adults in the United States. Annu Rev Public Health. 2022 Apr 5;43:503-523. doi: 10.1146/annurev-publhealth-052620-100313. Epub 2021 Dec 9. PMID: 34882432.
Unger CA. Hormone therapy for transgender patients. Transl Androl Urol. 2016 Dec;5(6):877-884. doi: 10.21037/tau.2016.09.04. PMID: 28078219; PMCID: PMC5182227.