How much blood is too much blood?
Have you ever found yourself wondering “is my period normal”?
From the moment we start bleeding, this question of “how much blood is too much blood?” seems to become a source of anxiety for most menstruators.
Sure, we’re aware that bleeding is normal when we’re on our periods, but knowing if our bleeding is heavy, irregular, or painful enough that we should see a doctor is a bit more complicated.
Between the overly metaphorical information we get from period product ads, and the confusing benchmarks that doctors and public health peeps share with us (how would we even measure how many ml or tablespoons of blood we lose every month?), it can be hard to know where to look for clear and reliable information about what counts as typical vs abnormal bleeding.
To make matters worse, we’re told from a young age that period pain is normal. Our discomfort is usually dismissed as “just bad cramps”, and we’re told to take a tylenol and “deal with it”.
These factors can make it difficult to find support. Luckily, Hormonally is here to be your heavy bleeding buddy and encourage you to find out more about what counts as abnormal, and how to find relief when you need it.
So keep reading to get the scoop on how to identify when your bleeding or pain is in need of investigation, why you might be experiencing these symptoms, and most importantly, what you can do about it.
Adding in ‘for me’
A tip that I suggest for answering your questions about bleeding and discomfort is to add a “for me” at the end of your queries. How much blood is too much blood for me? How much pain is too much pain for me?
Our bodies are all different, with our menstrual cycle lengths and baselines for discomfort varying. When you notice changes in your cycle length compared to what you’re used to, differences in the amount of blood or timing of your bleeding, or increased pain compared to the way you typically feel, this is when you should seek support.
While it’s not a perfect fix, especially if your period turns up whenever it feels like it, taking stock of how you feel is generally helpful.
Equally, if you’re facing a physician that tends to tell you that your experience is “perfectly normal”, remember that it’s OK to use this as a way to make your case. It’s OK to say “I know my body, and I know this isn’t normal for me”.

A (limited) guide to downstairs disturbances
If you bleed when you’re not on your period, or you have heavy or prolonged periods, you’re probably dealing with something called abnormal uterine bleeding (AUB).
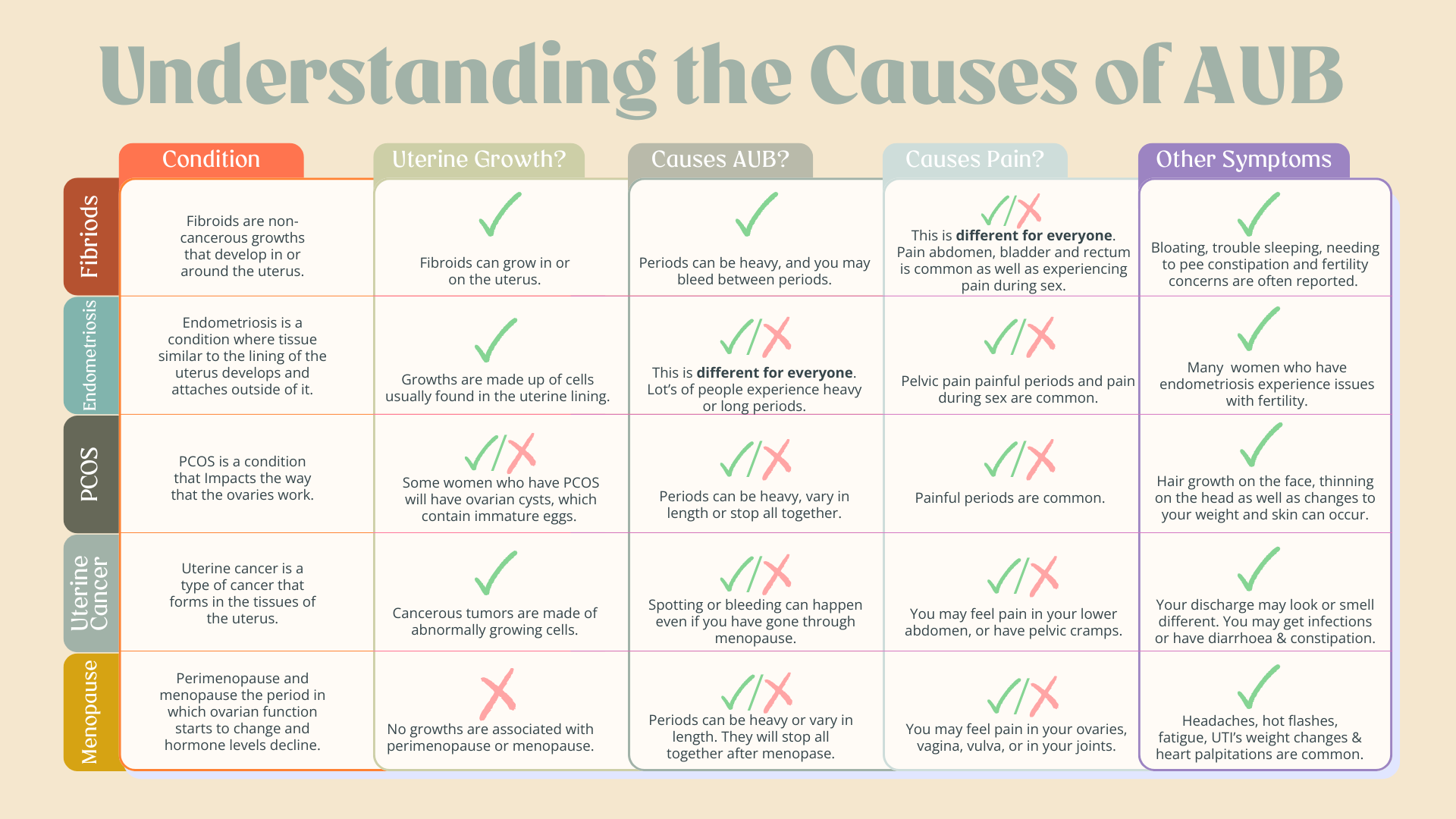
AUB can be caused by a range of gynecological conditions, so it’s important not to jump to conclusions about the conditions you think you might be experiencing if you have noticed AUB.
In an effort to minimize google-induced spiraling, I’ve put together a table that highlights key similarities and differences between some conditions that are known to be related to AUB.
Remember, if you’re experiencing any of the symptoms listed below, you should talk to your doctor. They’ll be able to assess your medical history and help you to understand what may be happening hormonally, using the right evidence based information. Based on your consultation, they’ll also be able to make suggestions as to how you could proceed with treatments.
.
It’s hard out here for women
Did you know that most women experience at least four reproductive health conditions over the course of their lives? And they can happen AT THE SAME TIME! For instance, you can go through menopause and have fibroids. Or, be struggling with endometriosis and have PMDD.
Unfortunately, we still don’t have a clear idea of why some women experience AUB while others are spared. There’s likely more than one explanation for this, and hormones definitely play a role, but another popular theory is that growths like fibroids, cysts, endometrial growths, and tumors can prevent the uterus from properly contracting.
The squeezing and tightening of our uteruses physically initiates bleeding, but these motions also act to control how much blood is lost, as well as how long bleeding lasts. Depending on the location, number, and size of growths that a woman has, this could create a physical barrier, preventing her uterus from contracting properly, leading to AUB.
Regardless of the cause, AUB can become a life-altering issue. This really stresses the importance of getting proper support. You know what they say, after all. No (wo)man is an island. We all need support, and we all need access to the right care that takes into account the full spectrum of our experiences.
What can I do about my AUB and pain?
Once you’ve figured out what the problem is, it’s time to do something about it!
First things first. If you experience heavy bleeding, you’ll want to get bloodwork done to check for iron deficiencies, as heavy bleeding can cause you to develop anemia. You should also take this opportunity to check your ferritin levels. Your iron levels may look normal, but ferritin – a protein that helps to manage iron in your body- may tell a different story!
Next it’s time to talk about treatment. Your doctor might suggest that you try birth control medications or think about having a hormonal intrauterine device (IUD) fitted to help address both pain and bleeding. These methods work by managing the levels of hormones produced in your ovaries.
Controlling these hormone levels helps to slow bleeding, and as a result can address the cramping experienced with heavy periods!
A medication called Elagolix is also an option your doctor may talk to you about. Elagolix is a type of treatment called a gonadotropin-releasing hormone (GnRH) antagonist, and it works by regulating the hormones linked to heavy bleeding.
Calling all AUB-ers!
As many as one in three women experience AUB globally, which is why it’s so important to make information available for us to explore how AUB may be affecting each of us differently.
Studies have shown that women who experience AUB tend not to get medical care. I’d bet that struggles in finding relevant information, in addition to the negative experiences that women often have when trying to report our symptoms, contributes to this trend.
Whatever the reason, it’s time to flip the script. Let’s normalize prioritizing our wellbeing.
If you find yourself among this group of women who experience heavy bleeding and pain, I hope that this blog post has cleared up some of your questions.
I also want to drive home the point that you know your body best. Doctors may go to school for years and know A LOT about how the human body works, but you have spent every single moment of your life in your own body. If you think something feels off, go with your gut and get it checked out.
In this bid to put ourselves and our wellness first, I’m calling on you to make that doctor’s appointment, insist on being taken seriously, and help get a handle on that AUB!

References
Gupta S, Jose J, Manyonda I. Clinical presentation of fibroids. Best Pract Res Clin Obstet Gynaecol. 2008;22(4):615-626. doi:10.1016/j.bpobgyn.2008.01.008
InformedHealth.org. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Overview: Heavy periods. [Updated 2021 Jun 17]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279294/
Makker V, MacKay H, Ray-Coquard I, et al. Endometrial cancer. Nat Rev Dis Primers. 2021;7(1):88. Published 2021 Dec 9. doi:10.1038/s41572-021-00324-8
Ndefo UA, Eaton A, Green MR. Polycystic ovary syndrome: a review of treatment options with a focus on pharmacological approaches. P T. 2013;38(6):336-355.
Nowak RA, Rein MS, Heffner LJ, Friedman AJ, Tashjian AH Jr. Production of prolactin by smooth muscle cells cultured from human uterine fibroid tumors. J Clin Endocrinol Metab. 1993;76(5):1308-1313. doi:10.1210/jcem.76.5.8496322
Parasar P, Ozcan P, Terry KL. Endometriosis: Epidemiology, Diagnosis and Clinical Management. Curr Obstet Gynecol Rep. 2017;6(1):34-41. doi:10.1007/s13669-017-0187-1
Whitaker L, Critchley HO. Abnormal uterine bleeding. Best Pract Res Clin Obstet Gynaecol. 2016;34:54-65. doi:10.1016/j.bpobgyn.2015.11.012






